Airborne diseases are illnesses that spread through tiny droplets or particles in the air. When an infected person coughs, sneezes, talks, or even breathes, germs are released and can stay in the air for minutes or even hours. Anyone nearby can inhale these germs and become sick. This is why airborne diseases spread quickly, especially in crowded, closed, or poorly ventilated environments like classrooms, offices, public transport, and hospitals.

People with weak immune systems, children, and older adults are at a higher risk of developing complications from airborne infections.
How Airborne Diseases Spread?
When a person is infected:
- Droplet Transmission: Larger droplets fall quickly to surfaces but can infect people within close distance.
- Aerosol Transmission: Very tiny particles stay suspended in the air for a long time and can travel longer distances.
Some germs also settle on objects, and touching these surfaces followed by touching the face or mouth can cause infection.
Also read about this: Airborne Diseases
Remember: https://healthytipspro.com/diabetes/
Common Airborne Diseases
Airborne diseases are caused by viruses and bacteria that travel through the air in tiny droplets when an infected person coughs, sneezes, talks, or breathes. These germs can remain suspended in the air for some time, making it easy for others nearby to inhale them and become infected. Below are some of the most common airborne diseases seen globally, especially in communities with crowded living spaces, poor ventilation, or weak healthcare systems.
Tuberculosis (TB):
Tuberculosis is a serious bacterial infection caused by Mycobacterium tuberculosis. It mainly affects the lungs and spreads when an infected person coughs or speaks, releasing bacteria into the air. Symptoms include a persistent cough, chest pain, fever, night sweats, and unintentional weight loss. People living in close contact with TB patients, smokers, and those with weak immune systems are at higher risk. TB requires a long course of antibiotics (usually 6 months or more), and treatment must be completed fully to prevent drug resistance.
Influenza (Flu):
Influenza is a viral infection that affects the respiratory system. It spreads easily in schools, offices, public transport, and crowded gatherings. Flu symptoms include high fever, sore throat, muscle aches, tiredness, and cough. While most people recover within a week, young children, pregnant women, elderly individuals, and people with chronic illnesses may develop severe complications. Vaccination and good hygiene are key to prevention.
COVID-19:
Caused by the coronavirus SARS-CoV-2, COVID-19 spreads through both droplets and airborne particles. Symptoms range from mild cold-like illness to severe pneumonia, depending on individual health. Common signs include fever, cough, fatigue loss of taste or smell, and breathing difficulty. Vaccination, masks, ventilation, and early medical care help reduce severe outcomes.
Common Cold:
The common cold, usually caused by rhinoviruses, is among the most frequent airborne infections. It leads to runny nose, sneezing, mild fever, sore throat, and fatigue. Although usually mild, it spreads quickly through schools and workplaces. Rest, hydration, and home care are generally enough for recovery.
Measles:
Measles is a highly contagious viral infection that spreads through the air when an infected person breathes, talks, or coughs. It can stay suspended in the air for up to two hours. Symptoms include high fever, cough, red eyes, and a widespread skin rash. Measles can lead to serious complications, especially in children, but it is preventable through vaccination (MMR vaccine).
Chickenpox:
Chickenpox is caused by the varicella-zoster virus and spreads through airborne droplets and direct contact with infected blisters. It usually causes itchy fluid-filled blisters, fever, and fatigue. While mostly mild in children, it can be severe in adults or people with weakened immunity. Vaccination is the best prevention.
Whooping Cough (Pertussis):
Pertussis is a bacterial infection caused by Bordetella pertussis. It is known for severe coughing fits that end with a “whooping” sound as the person tries to breathe in. Infants are at the highest risk. Vaccination (DTaP or Tdap) helps prevent this disease.
Common Symptoms of Airborne Infections
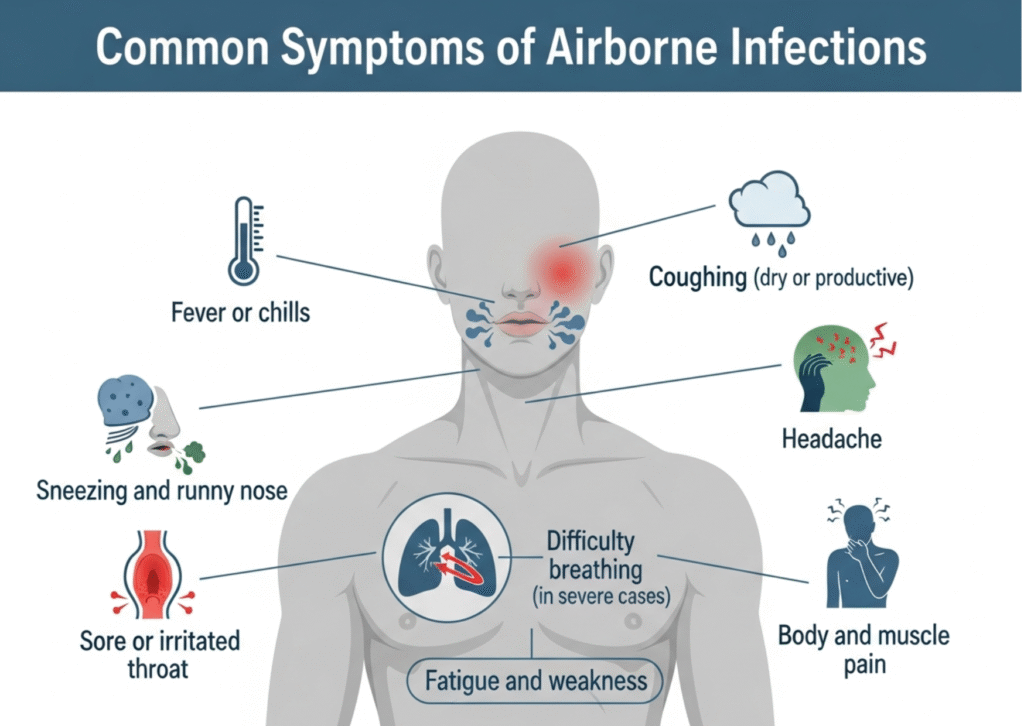
Many airborne diseases share similar symptoms:
- Fever or chills
- Coughing (dry or productive)
- Sneezing and runny nose
- Sore or irritated throat
- Headache
- Body and muscle pain
- Fatigue and weakness
- Difficulty breathing (in severe cases)
If symptoms worsen or breathing becomes difficult, seek medical care immediately.
Diagnosis
Doctors may use:
- Physical Examination
- Chest X-ray or CT scan (especially for TB or pneumonia)
- Blood Tests
- PCR Tests (for viruses like COVID-19 or Flu)
- Sputum Culture Tests (for Tuberculosis)
Early diagnosis prevents complications and stops the spread.
Treatment Methods of Common Airborne Diseases
Rest & Proper Sleep
Adequate rest allows the immune system to fight infections effectively. Sleep reduces physical stress and helps control inflammation, supporting faster recovery.
Hydration (Water, Soups, ORS)
Keeping the body hydrated is essential, especially when fever causes fluid loss. Water, warm soups, and ORS (Oral Rehydration Solution) help maintain electrolyte balance and prevent dehydration.
Fever & Pain Control (Paracetamol, Ibuprofen)
Medications like Paracetamol or Ibuprofen help lower fever, ease headaches, body aches, and provide comfort during recovery. These should be used as per medical advice.
Antivirals (If Prescribed)
In viral infections such as Influenza or COVID-19, doctors may prescribe antiviral medications to reduce symptom severity and shorten the duration of illness. These medicines work best when taken early.
Antibiotics (When Bacterial Infection Is Confirmed)
Antibiotics are not useful for viral infections, but they are essential when the illness is caused by bacteria, such as Tuberculosis or Whooping Cough. Proper dosing and completing the full course is important to prevent drug resistance.
Hospitalization for Severe Cases
If breathing becomes difficult, oxygen levels drop, or high fever does not improve, hospital care may be required. Hospitals provide oxygen therapy, IV fluids, and close monitoring to prevent complications.
Long-Term TB Treatment (6+ Months)
Tuberculosis requires long-term treatment, usually6 months or more, using a combination of specific antibiotics. Completing the entire course is crucial to avoid drug-resistant TB, which is harder to treat.
This structured approach ensures effective recovery, prevents complications, and reduces the spread of airborne diseases within families and communities.
Prevention & Control
You can reduce the risk of airborne diseases by practicing:
- Wear a mask in crowded or indoor public places
- Wash hands frequently with soap
- Keep rooms well-ventilated
- Avoid close contact with sick people
- Cover mouth & nose when coughing or sneezing
- Clean frequently touched surfaces
- Get vaccinated (Measles, Flu, COVID-19, etc.)
- Eat a balanced diet to strengthen immunity
Diet Chart for Airborne Disease Recovery (Daily Meal Plan)
| Meal Time | What to Eat | Why It Helps |
| Early Morning | Warm water with lemon OR Honey + Ginger warm water | Helps soothe throat, reduce inflammation, boosts immunity. |
| Breakfast | Oatmeal / Porridge with milk OR Boiled eggs + Whole wheat bread OR Vegetable upma / khichdi | Provides energy, easy to digest, boosts strength. |
| Mid-Morning Snack | Fresh fruits like banana, apple, papaya, orange OR Coconut water | Restores vitamins, maintains hydration, supports immune system. |
| Lunch | Roti / Rice + Dal + Cooked vegetables + A small salad | Balanced meal provides proteins, fiber, and essential nutrients. |
| Evening Snack | Vegetable soup / Chicken soup / Lentil soup | Keeps the body warm, helps relieve cough & improves immunity. |
| Dinner | Light meal: Khichdi / Vegetable stew / Soft chapati with dal | Easy to digest and prevents digestive stress during illness. |
| Before Bed | Warm turmeric milk (Haldi Doodh) or Chamomile tea | Reduces inflammation and supports restful sleep for recovery. |
Recommended Foods
- Warm soups (vegetable, chicken, lentil)
- Fresh fruits (rich in Vitamin C: oranges, guava, strawberries)
- Green leafy vegetables (spinach, broccoli)
- Protein foods (eggs, fish, lentils, beans)
- Yogurt / Curd (supports gut immunity)
- Herbal teas: ginger tea, tulsi tea, honey + warm water
Foods to Avoid
| Avoid | Why |
| Cold drinks / Ice creams | Increase congestion and throat irritation. |
| Fried & oily foods | Slow digestion and weaken immunity. |
| Excess sugar & sweets | Increases inflammation and slows recovery. |
| Spicy foods | Can worsen cough and throat irritation. |
| Processed & packaged snacks | Low nutrition, weakens body defense. |
Doctors’ Roles in Managing Airborne Diseases
| Type of Doctor | Role in Treatment | When to Consult |
| General Physician / Family Doctor | Performs initial examination, checks symptoms, prescribes fever and pain medicines, and monitors basic recovery. | When symptoms like fever, cough, or sore throat first appear. |
| Pulmonologist (Lungs Specialist) | Diagnoses and treats lung-related diseases like TB, pneumonia, asthma, and severe respiratory infections. Conducts chest X-rays, pulmonary tests, and advanced treatment. | If cough lasts more than 2–3 weeks, difficulty breathing, chest pain, or chronic lung infection suspected. |
| Infectious Disease Specialist | Handles severe, contagious, or complicated infections (TB, COVID-19, Whooping Cough). Guides antibiotic or antiviral treatment plans. | When infection is severe, recurrent, or drug resistance is suspected. |
| Pediatrician (Child Specialist) | Treats airborne diseases in children such as measles, flu, pneumonia, and whooping cough. Guides vaccination schedule. | If a child develops fever, rash, cough, or breathing difficulty. |
| Respiratory Therapist / Hospital Care Team | Provides oxygen therapy, nebulization treatments, airway clearance, and respiratory support in hospitals. | During severe breathing problems or hospitalization cases. |
Conclusion
Airborne diseases spread easily because germs travel freely in the air, especially in crowded and closed environments. Awareness, early diagnosis, complete treatment, and preventive measures like mask-wearing, hand hygiene, and vaccination play a major role in controlling these diseases. By protecting ourselves and being considerate of others, we can create healthier homes, schools, workplaces, and communities.
Appoint Doctor:
If you or someone has symptoms like continuous cough, fever, breathing difficulty, or chest pain, it is important to consult: Click Now Pulmonologist
How do airborne diseases spread from one person to another?
Airborne diseases spread when an infected person coughs, sneezes, talks, or even breathes, releasing tiny droplets or particles into the air. These germs can stay in the air and be inhaled by others, especially in closed or crowded places.
What are the first common symptoms of airborne infections?
Early symptoms usually include cough, fever, sore throat, runny nose, headache, fatigue, and body pain. In severe cases, there may be difficulty breathing or chest discomfort, especially in conditions like COVID-19, pneumonia, or TB.
Can airborne diseases be prevented by wearing a mask?
Yes. Wearing a mask reduces the chance of breathing in infected droplets and also prevents spreading germs to others. Masks are especially useful in public places, hospitals, classrooms, offices, and during outbreaks.
Do antibiotics work for all airborne diseases?
No. Antibiotics only work for bacterial infections (like Tuberculosis or Whooping Cough). They do not work for viral infections like Flu, COVID-19, Measles, or Common Cold. Viral infections need rest, hydration, and sometimes antiviral medications, not antibiotics.
Who is most at risk of severe airborne diseases?
People with weak immune systems are at higher risk, including:
Children
Elderly
Pregnant women
Those with diabetes, heart disease, or lung disease
Smokers
People living in crowded or poor-ventilated areas
Keeping immunity strong and practicing hygiene can reduce the risk.
Pingback: Insect Born Diseases-A Complete Guide